
#Rectal gonorrhea symptoms trial#
This was a secondary analysis of data from a cross sectional MSM survey conducted at a multisite randomized controlled trial (RCT) (December 2018 to January 2019) around uptake of gonorrhea and chlamydia testing among Chinese MSM (N = 431). We evaluate whether Chinese MSM select an STI test (rectal vs urethral) appropriate for their sexual behavior (insertive and/or receptive), and the interactions with being out. MSM do not frequently receive rectal STI testing because of several barriers, such as not being out (disclosure of sexual behavior). Men who have sex with men (MSM) globally have a high burden of curable sexually transmitted infections (STIs). We conclude by discussing future directions in HIV prevention research in light of forthcoming technologies such as fifth generation (5G) mobile networks, combined use of self-collected biological data alongside self-report, and the utility of metadata and metaresearch to document, evaluate, and inform best practices. In this article, we discuss methodological considerations for using the internet to conduct HIV prevention research with MSM: (1) sources of recruitment (eg, geosocial apps, Facebook, crowdsourced online panels) (2) design (eg, cross sectional, longitudinal, diaries) (3) incentives (including disincentivizing fraudulent participants and/or spam bots) (4) confidentiality and (5) representativeness. In tandem, researchers have rapidly expanded their employment of internet-mediated methods for the recruitment and engagement of key populations for HIV research, treatment, and prevention. Notable transitions include MSM's expanded use of geosocial networking apps, as well as other forms of social media accessed primarily through mobile devices, as well as the addition of biomedical prevention strategies (eg, pre-exposure prophylaxis and undetectable = untransmittable) to the proverbial HIV prevention toolkit. In this article, we discuss historical events and research having occurred in the half decade since the Grov et al publication. In 2014, Grov et al published a comprehensive review cataloguing both men who have sex with men's (MSM's) sexual behavior transitions in online environments from the 1990s through 2013, as well as researchers' efforts in tandem to use the internet to engage MSM into research, treatment, and prevention.

#Rectal gonorrhea symptoms full#
Our finding that insertive CAS acts was associated with rectal GC/CT highlights that providers should screen patients for GC/CT via a full range of transmission routes, lest GC/CT go undiagnosed.
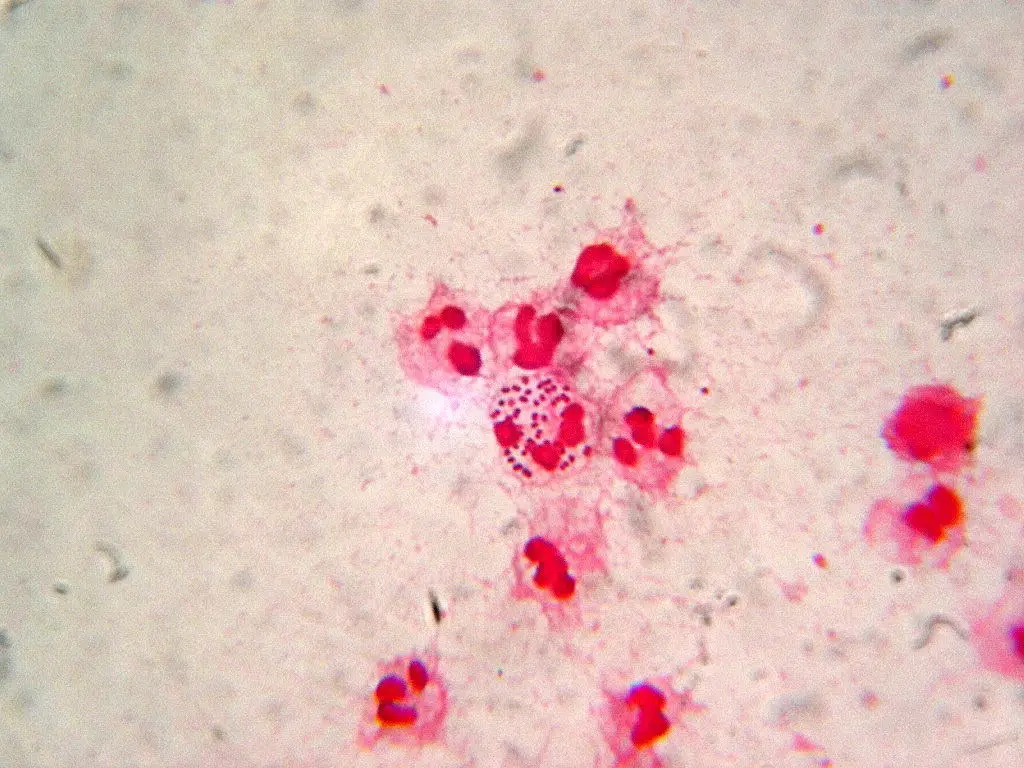
Rectal GC/CT was more common than urethral and associated with some demographic and behavioral characteristics. The number of male partners (<12 months) was associated with increased odds of urethral GC/CT. Compared with those who had engaged in both insertive and receptive anal sex, those who engaged in only receptive anal sex had lower odds of urethral GC/CT. There was a positive association between rectal GC/CT and number of male partners (<12 months), the number of anal receptive acts, receptive condomless anal sex (CAS) acts, and insertive CAS acts. Among men who reported anal sex, those reporting only insertive sex had lower odds of rectal GC/CT than did men who reported both insertive and receptive. Compared with white men, Latinos had significantly greater odds of rectal GC/CT. Age was inversely associated with urethral and rectal GC/CT. We calculated adjusted (for education, race, age, relationship status, having health insurance, and income) odds ratios for factors associated with rectal and urethral GC/CT diagnoses. In total, 6.2% were GC/CT positive (5.3% rectal, 1.7% urethral). Rectal GC/CT symptoms may be less obvious than urethral, increasing opportunities for undiagnosed rectal GC/CT.Ī US national sample of 1071 gay and bisexual men completed urethral and rectal GC/CT testing and an online survey. Gay and bisexual men are at elevated risk for Neisseria gonorrhoeae and Chlamydia trachomatis (GC/CT).


 0 kommentar(er)
0 kommentar(er)
